Recognizing Perioperative Tachycardia
Recognizing Perioperative Tachycardia
Blog Article
Perioperative tachycardia, a common occurrence in surgical procedures and the immediate after period, presents a concern for healthcare professionals. It refers to a rapid heart rate exceeding a predetermined threshold, typically classified as 100 beats per minute or more. This condition can arise due to a variety of factors, such as physiological stress, anxiety, pain, and underlying medical conditions. Understanding the causes and potential implications of perioperative tachycardia is vital for providing optimal patient care.
Early identification and management are essential to minimize potential adverse events. Healthcare providers should frequently assess patients' heart rates during the perioperative period and implement appropriate interventions, such as medication administration, to restore hemodynamic stability.
Addressing Postoperative Tachycardia: A Clinical Guide
Postoperative tachycardia, a frequently observed complication following surgery, can present significant challenges for clinicians. This phenomenon is characterized by an elevated heart rate which typically remains elevated a prolonged period post-procedure.
Understanding the underlying mechanisms of postoperative tachycardia is crucial for establishing effective management strategies. Various factors can contribute to this state, including pain, anxiety, fluid depletion, and autonomic nervous system instability.
Effective treatment of postoperative tachycardia involves a multimodal approach. Medication-based often play a central role, with options such as beta-blockers and calcium channel blockers employed to regulate heart rate. Alongside medication therapy, physical therapies can be helpful. These may include stress reduction techniques, optimization of pain management, and appropriate fluid replacement.
A comprehensive assessment of the patient's clinical status, with consideration to their medical history, current medications, and postoperative course, is essential for adjusting the management plan. Close monitoring of vital signs, including heart rate, blood pressure, and oxygen saturation, is crucial to maintain patient safety and effectively manage postoperative tachycardia.
Perioperative Heart Rate Elevation: Causes and Considerations
Elevated heart rates during the perioperative period can occur as a common physiological response to various factors. A myriad of causes can contribute this phenomenon, ranging from anesthetic agents and operative stress to underlying cardiovascular conditions.
It's essential for clinicians to thoroughly assess the root cause of perioperative heart rate elevation, as it can affect patient outcomes and inform management strategies. A comprehensive history should include a detailed review of the patient's anesthetic history, preoperative vital signs, and current medications.
Furthermore, physical examination findings can provide valuable insights regarding potential underlying issues.
Is Tachycardia After Surgery Normal? Exploring Common Causes
Following a surgical procedure, a person's heart rate may often increase. This accelerated heartbeat, known as tachycardia, can be a frequent occurrence in the postoperative period. However, understanding the underlying causes of tachycardia after surgery is essential for timely diagnosis and treatment. Some frequent culprits include pain, anxiety, dehydration, medications, and a drop in blood volume. In many cases, tachycardia resolves on its own as the body recovers.
However, if you are observing persistent or alarming tachycardia after surgery, it's critical to consult with your healthcare provider immediately.
The Incidence and Impact of Perioperative Tachycardia
Perioperative tachycardia presents in a significant proportion of patients undergoing surgical procedures. This condition, characterized by an elevated heart rate during surgery, can have a pronounced impact on patient outcomes. The exact incidence of perioperative tachycardia varies depending on factors such as the type of surgery, anesthetic techniques employed, and the patient's underlying surgical conditions.
Increased heart rates can cause hemodynamic instability, leading to complications such as hypotension, arrhythmias, and myocardial ischemia. Furthermore, perioperative tachycardia has been associated with an increased risk of postoperative mortality.
Recognizing the potential consequences, clinicians must actively monitor heart rate during the perioperative period and implement strategies to control tachycardia when required.
Tachycardia in the Operating Room: Assessment and Management
Tachycardia in the operating room can signal a critical hemodynamic disturbance. A rapid heart rate requires prompt identification and suitable management to guarantee patient well-being.
The initial step involves a thorough comprehensive examination, including assessing vital signs like heart rate, blood tension, and respiratory rate.
A detailed history of the patient's past medical condition should in addition be obtained to determine potential contributing factors.
Heart monitoring is essential to confirm the nature of tachycardia and recognize any irregularities.
Blood tests may be useful in evaluating electrolyte imbalance, thyroid function, and other elements that could be affecting to the tachycardia.
Based on the evaluation, management tactics should be adjusted to the primary cause and the patient's overall condition.
Treatment options may comprise fluid infusion, sodium adjustment, medication administration to control heart rate and rhythm, and in some cases, invasive procedures such as synchronized electrical stimulation.
Continuous monitoring of the patient's vital signs and reaction to treatment is crucial throughout the perioperative period.
Factors Influencing Perioperative Heart Rate Dynamics
Perioperative heart rate dynamics are significantly influenced by a complex interplay of biologic factors. Preoperative patient characteristics such as age, preexisting medical conditions, and anxiety levels can contribute to resting pulse. Intraoperatively, anesthetic agents, surgical stimulation, and hemodynamic adjustments can influence heart rate. Postoperatively, pain, inflammation, and restitution also play a role in pulse patterns. Careful monitoring and adaptation of these factors are crucial to ensure optimal cardiovascular outcomes during the perioperative period.
Post-Operative Tachycardia
Post-operative tachycardia, characterized by an accelerated heart rate following surgery, can significantly/noticeably/potentially impact patient recovery. This condition can manifest as a result of various factors, including anesthesia, pain, and inflammation. While often temporary, persistent tachycardia may indicate/suggest/point to underlying complications, necessitating prompt/timely/immediate medical attention. Monitoring heart rate closely after surgery is crucial/essential/vital to ensure optimal healing and minimize potential risks associated with this common/frequent/usual postoperative phenomenon.
Perioperative Arrhythmias: Recognizing and Addressing Tachycardia
During the perioperative period, patients are at risk to developing arrhythmias. One of the frequently encountered types is tachycardia, characterized by a heart rate greater than normal limits. Prompt recognition and management of tachycardia are essential to patient safety. Physiological signs may include palpitations, shortness of breath, chest pain, dizziness, or fainting. An ECG is the most important tool for identifying tachycardia. Treatment approaches depend on the underlying cause and severity of the arrhythmia. Medications options include beta-blockers, calcium channel blockers, and antiarrhythmic agents.
In some cases, interventional procedures such as cardioversion or catheter ablation may be indicated.
Strategies for Minimizing Perioperative Tachycardia
Minimizing perioperative tachycardia requires a multifaceted approach that encompasses various pre-, intra-, and postoperative interventions.
A comprehensive evaluation of the patient's medical history, including underlying conditions and medications, is crucial for identifying potential risk factors contributing to tachycardia.
Preoperative optimization strategies such as judicious fluid management, electrolyte balance correction, and anxiolysis can help mitigate autonomic activation.
During surgery, attenuating the hemodynamic stress response through careful anesthetic techniques, adequate analgesia, and temperature control is essential. Maintaining a calm and supportive environment for the patient can also contribute to reducing tachycardia.
Postoperatively, vigilant monitoring, early ambulation, and pain management are essential in facilitating regeneration and preventing post-operative complications.
Heart Rate Variability During Surgery: Insights into Cardiac Stress
During surgical procedures, patients often experience physiological tension. This can lead to alterations in various bodily functions, including heart rate variability (HRV). HRV, a measure of the variation in time between consecutive heartbeats, provides valuable insights into the autonomic nervous system's engagement. Reduced HRV during surgery has been associated with increased probability of adverse events.
Physicians and researchers utilize HRV monitoring as a potential tool to assess cardiac performance during surgery. By analyzing the patterns of HRV, clinicians can gain a better appreciation of the patient's neurological state. This get more info information can be instrumental in adjusting surgical strategies and ensuring optimal patient care.
- Moreover, HRV monitoring may serve as an early signal of impending cardiac issues during surgery, allowing for timely treatment to mitigate potential risks.
- However, the relationship between HRV and surgical stress is complex, requiring further investigation to fully elucidate its implications in clinical practice.
Perioperative Tachycardia Control: The Role of Anesthesia
Perioperative tachycardia presents a common challenge for medical professionals. Prompt and effective management is crucial to minimize adverse outcomes and ensure patient stability. Anesthesiologists utilize a variety of techniques, including pharmacologic agents like antiarrhythmics, to regulate heart rate during both the induction and maintenance phases of anesthesia. Furthermore, optimizing anesthetic depth and monitoring hemodynamics closely are essential components of tachycardia mitigation. By implementing these strategies, anesthesiologists can effectively manage perioperative tachycardia and contribute to a successful surgical outcome.
Preoperative Risk Factors for Postoperative Tachycardia
Identifying subjects at risk for postoperative tachycardia is crucial for optimizing perioperative care. Several preoperative characteristics can contribute to this complication. Increased age is a significant risk factor, as the cardiovascular system may present greater stress during and after surgery. Concurrent conditions such as hypertension, diabetes mellitus, and coronary artery disease can in addition amplify the probability of postoperative tachycardia. Furthermore, certain anesthetic agents and surgical procedures inherently carry a risk for tachycardia.
- Anteoperative medication use, particularly beta-blockers or anticholinergics, can also modify the risk of postoperative tachycardia. Individuals who are smokers may be more susceptible to this issue due to nicotine's effects on heart rate and rhythm.
Preemptive Treatment Strategies for Perioperative Arrhythmias
Perioperative tachycardia, a common cardiovascular complication in surgical procedures, can have adverse consequences for patient outcomes. Immediate detection and intervention are crucial to reduce the risk of complications like myocardial ischemia, arrhythmias, and hemodynamic instability. Clinicians should implement a multi-pronged approach that encompasses continuous cardiac monitoring, meticulous intraoperative management, and timely pharmacological interventions. Additionally, patient education regarding surgical risk factors and strategies to improve cardiovascular health can contribute to a less risky surgical experience.
Optimizing Fluid Management to Prevent Tachycardia After Surgery
Maintaining hemodynamic stability after surgery is crucial for patient recovery. One key aspect of this management involves optimizing fluid administration to prevent tachycardia. excessive fluid shifts can trigger an elevation in heart rate, potentially leading to complications. Therefore, meticulous monitoring of fluid input and output is essential. A balanced approach, considering factors such as patient age, pre-operative status, and surgical procedure, will help clinicians ensure appropriate hydration levels. Close collaboration between the anesthesia team and the surgical team is essential to execute a tailored fluid management strategy that minimizes the risk of postoperative tachycardia.
Perioperative Tachycardia: Influence on Surgical Outcomes
Perioperative tachycardia, a common physiological response during surgical procedures, has been shown to potential unfavorable outcomes. While some degree of tachycardia is anticipated in the perioperative period, prolonged elevations in heart rate can contribute various surgical issues. Studies have demonstrated a correlation between perioperative tachycardia and increased risk of postoperative complications such as wound infection, heart problems, and prolonged hospital stay.
The underlying causes contributing to perioperative tachycardia are multifactorial and can include anesthetic agents, pain, stress, hypoxia, and autonomic nervous system imbalance. Recognizing patients at increased risk for perioperative tachycardia is crucial for implementing appropriate strategies to mitigate its potential unfavorable implications. Early detection and management of tachycardia can improve surgical outcomes, reduce postoperative morbidity, and enhance patient recovery.
Patient-Specific Factors Influencing Postoperative Heart Rate
A multitude of patient-specific factors can significantly influence postoperative heart rate. These factors encompass age, preexisting medical conditions, and drug regimens the patient is using. Additionally, psychological factors such as anxiety can impact an elevated heart rate following surgery. Patients who are more conditioned may exhibit a more rapid recovery and as a result a quicker return to baseline heart rate. Conversely, patients possessing issues during or after surgery may experience a prolonged increase in heart rate. Understanding these patient-specific variables is crucial for clinicians to evaluate postoperative heart rate and apply appropriate interventions to ensure optimal patient care.
Postoperative Tachycardia
Tachycardia is/can be/presents as a common complication/occurrence/issue in the post anesthesia care unit PACU. It refers to/describes/indicates a heart rate above/exceeding/greater than 100/120/140 beats per minute bpm. Several factors/A variety of etiologies/Multiple contributors can contribute/lead to/cause tachycardia in the PACU, including/such as/among which are residual anesthetic effects, pain, anxiety, dehydration, hypovolemia, and electrolyte imbalances/disruptions/disturbances. Early identification/Prompt recognition/Detecting tachycardia is crucial/essential/important to ensure/guarantee/facilitate patient safety. Clinicians should/must/are required to monitor heart rate closely and implement/utilize/apply appropriate interventions such as/including/in cases of fluid resuscitation, medications, and addressing underlying causes/factors/origins.
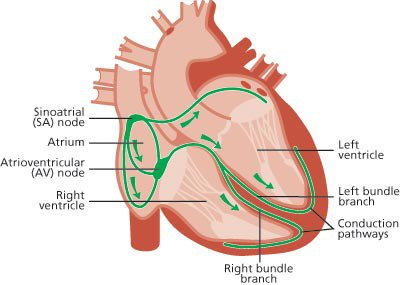
The Autonomic Nervous System and Postoperative Tachycardia
Perioperative tachycardia, a common occurrence during surgical procedures, results from the interplay between the sympathetic and parasympathetic divisions of the sympathovagal system. These branches dynamically regulate physiological processes to maintain homeostasis. During surgery, various factors such as anesthesia administration, surgical stimuli, and emotional stress can precipitate sympathetic activation, leading to an acceleration in heart rate. Conversely, parasympathetic activity may diminish, contributing to the overall tachycardia. Understanding this complex interplay is crucial for effective perioperative management and minimizing adverse outcomes.
Perioperative Tachycardia Monitoring Techniques
Effective management of tachycardia during the perioperative period requires meticulous monitoring strategies. Clinicians implement a variety of techniques to detect increased heart rates, which can signify underlying conditions.
Continuous electrocardiogram (ECG) monitoring provides real-time visualization of cardiac rhythm and rate. Oxygen saturation monitoring can also detect tachycardia by measuring pulse rate alongside oxygen saturation levels. Invasive hemodynamic measures, such as arterial blood pressure and central venous pressure, can provide additional insights about the cardiovascular condition.
Prompt detection of tachycardia allows for timely interventions to stabilize heart rate and prevent potentially life-threatening complications.
Report this page